Background: Long-term survival after intensive induction chemotherapy in acute myeloid leukemia (AML) is limited by both early mortality and disease resistance. A central clinical challenge is predicting which patients will experience early toxicity during induction or resistant disease. Limitations of prior analyses include a specific focus on either early treatment-related mortality or overall survival (OS), an absence of genetic annotation in early mortality studies, and reliance on clinical trial cohorts which may not be broadly representative. Here, we perform a detailed analysis of pretreatment clinical and disease characteristics in a cohort of real-world AML patients to elucidate factors associated with early mortality and with OS after induction.
Methods: We identified 290 consecutive adult patients treated with standard induction chemotherapy ("7+3" with cytarabine and an anthracycline, or CPX-351) for newly diagnosed AML (2014-2019). We collected pretreatment clinical, pathology, and laboratory data, and annotated clinical outcomes. Gene mutations were determined at the time of diagnosis using targeted next-generation sequencing of recurrently mutated genes. The median age at diagnosis was 61 years (range 19-76), with 56% of patients aged 60 or older. Most patients (71%) had de novo AML; 15% had clinically defined secondary AML and 14% had therapy-related AML. Median follow-up for survivors landmarked at 60 days was 26.1 months, with a minimum follow up of at least 60 days for all patients. Median OS and relapse-free survival (RFS), both landmarked at day 60, were 33.9 months and 28.0 months, respectively.
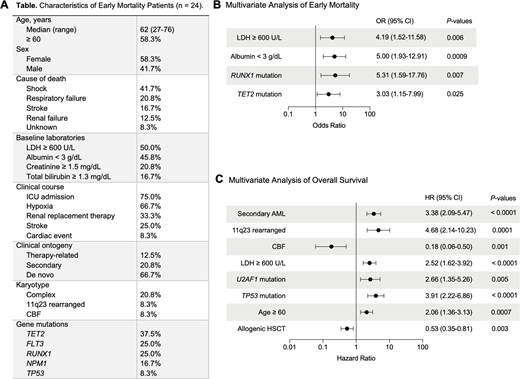
Results: In total, 24 of 290 (8%) patients died within the first 60 days of receiving induction chemotherapy, with shock being the most common cause of death (42%), followed by respiratory failure (21%) (Figure 1A). In a multivariable logistic regression model, we found that pretreatment albumin < 3 mg/dL, pretreatment LDH >= 600 U/L, and mutations in TET2 or RUNX1 were independently associated with death within 60 days (Figure 1B). Factors not independently associated with early mortality included older age (<60 versus 60 or older), clinical ontogeny (secondary or treatment-related AML), complex karyotype, and pretreatment blood counts.
To identify factors associated with outcomes among patients surviving past 60 days, we generated a multivariable model with allogeneic stem cell transplantation as a time-varying covariate. In this model, age >= 60, secondary AML, pretreatment LDH >= 600 U/L, and the presence of TP53 mutation, U2AF1 mutation, or 11q23 rearrangement were independently associated with inferior OS after day 60, whereas the presence of CBF rearrangement was independently associated with superior OS after day 60 (Figure 1C). To determine the contribution of resistant disease to OS landmarked at day 60, we developed multivariable models for failure to achieve remission by day 60 and for RFS landmarked at day 60, and then applied them to the OS model. All variables remained significant, indicating that disease resistance is a main driver of OS after 60 days.
Conclusions: Early treatment-related mortality is most commonly the result of shock and respiratory failure, irrespective of disease status, and is associated with specific pretreatment lab values (elevated LDH, low albumin) and disease-specific mutations (TET2 and RUNX1). Among patients surviving induction, survival is driven primarily by resistant disease (primary refractoriness and disease relapse) and is associated with factors previously correlated with outcome in AML, including age, clinical ontogeny, and disease genetics. Overall, we show that early and late outcomes in AML are associated with distinct sets of pretreatment clinical, genetic, and laboratory characteristics and for the first time show that disease-specific mutations are associated specifically with induction toxicity. Improved ability to identify patients likely to experience toxicity after receiving anthracycline-based AML induction may help develop mitigation strategies for these patients.
Figure 1: Predictors of early mortality and overall survival in AML patients undergoing induction.A. Clinical and genetic characteristics of early mortality patients. B-C. Forest plots of multivariate analysis of pretreatment risk factors associated with early mortality (B) and with OS landmarked at 60 days (C).
Lindsley:Jazz Pharmaceuticals: Consultancy, Research Funding; Takeda Pharmaceuticals: Consultancy; MedImmune: Research Funding; Bluebird Bio: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal